Abstract
Purpose
The purpose of this study was to examine the incidence of psychological complaints and the relationship of these complaints with the quality of life (QOL) and accident- and patient-related factors among severely injured patients after the rehabilitation phase.
Methods
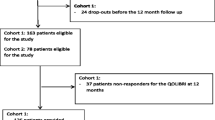
Patients of 18 years or older with an injury severity score above 15 were included 15–53 months after their accident. Accident and patient characteristics were obtained from questionnaires and the trauma registry. Several questionnaires (Hospital Anxiety and Depression Scale, Impact of Events Scale, and Cognitive Failure Questionnaire) were used to determine the symptoms of psychological problems (anxiety or depression, post-traumatic stress disorder, or subjective cognitive complaints, respectively). The World Health Organization Quality of Life-Bref was used to determine QOL. A reference group of the Dutch general population was used for comparison of QOL scores.
Results
The participation rate was 62 % (n = 173). At the time of the study, 30.1 % (n = 52) of the investigated patients had psychological complaints. No relation between psychological complaints and somatic severity or type of injury was found. Patients who were employed before the accident or resumed working reported less psychological complaints. Use of any medication before the accident and treatment for pre-accidental psychological problems were positively related to psychological complaints afterwards. QOL of severely injured patients was impaired in comparison with the general Dutch population, but only for those with psychological complaints.
Conclusions
Psychological complaints seem to be an important and underestimated factor for a decreased QOL among severely injured patients.


Similar content being viewed by others
References
Sluys, K., Haggmark, T., & Iselius, L. (2005). Outcome and quality of life 5 years after major trauma. Journal of Trauma, 59, 223–232.
Ringburg, A. N., Polinder, S., van Ierland, M. C., Steyerberg, E. W., van Lieshout, E. M., Patka, P., et al. (2011). Prevalence and prognostic factors of disability after major trauma. Journal of Trauma, 70(4), 916–922.
Holbrook, T. L., Anderson, J. P., Sieber, W. J., Browner, D., & Hoyt, D. B. (1999). Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. Journal of Trauma, 46, 765–771.
Alves, A. L., Salim, F. M., Martinez, E. Z., Passos, A. D., De Carlo, M. M., & Scarpelini, S. (2009). Quality of life in trauma victims six months after hospital discharge. Revista de Saude Publica, 43, 154–160.
Sutherland, A. G., Alexander, D. A., & Hutchison, J. D. (2006). The mind does matter: Psychological and physical recovery after musculoskeletal trauma. Journal of Trauma, 61, 1408–1414.
Baranyi, A., Leithgob, O., Kreiner, B., Tanzer, K., Ehrlich, G., Hofer, H. P., et al. (2010). Relationship between posttraumatic stress disorder, quality of life, social support, and affective and dissociative status in severely injured accident victims 12 months after trauma. Psychosomatics, 51(3), 237–247.
Michaels, A. J., Madey, S. M., Krieg, J. C., & Long, W. B. (2001). Traditional injury scoring underestimates the relative consequences of orthopedic injury. Journal of Trauma, 50, 389–395.
Bombardier, C. H., Fann, J. R., Temkin, N. R., Esselman, P. C., Barber, J., & Dikmen, S. S. (2010). Rates of major depressive disorder and clinical outcomes following traumatic brain injury. Journal of the American Medical Association, 303(19), 1938–1945.
Di, G. A., & Parry-Jones, W. L. (1996). Psychological sequelae of road traffic accidents: An inadequately addressed problem. British Journal of Psychiatry, 169(4), 405–407.
Ward, C. L., Flisher, A. J., Zissis, C., Muller, M., & Lombard, C. (2001). Exposure to violence and its relationship to psychopathology in adolescents. Injury Prevention, 7(4), 297–301.
Hays, R. D., Sherbourne, C. D., & Mazel, R. M. (1993). The RAND 36-Item Health Survey 1.0. Health Economics, 2(3), 217–227.
McHorney, C. A., Ware, J. E., Jr., & Raczek, A. E. (1993). The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31(3), 247–263.
Van der Zee, K. I., & Sanderman, R. (1993). Het meten van de algemene gezondheidstoestand met de RAND-36 [Measuring health status with the RAND-36]. Groningen: Rijksuniversiteit Groningen.
De Vries, J. (2001). Quality of life assessment. In A. D. Vingerhoets (Ed.), Assessment in behavioral medicine (pp. 353–370). Hove: Psychology Press.
(1995). The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Social, Science & Medicine, 41(10), 1403–1409.
Hamming, J. F., & De Vries, J. (2007). Measuring quality of life. British Journal of Surgery, 94(8), 923–924.
van Delft-Schreurs, C. C., van Bergen, J. J., de Jongh, M. A., van de Sande, P., Verhofstad, M. H., & De Vries, J. (2013). Quality of life in severely injured patients depends on psychosocial factors rather than on severity or type of injury. Injury, S0020–S1383.
Association for the Advancement of Automotive Medicine (AAAM). (1998). The Abbreviated Injury Scale 1990 revision—update 98.
Baker, S. P., O’Neill, B., Haddon, W., Jr., & Long, W. B. (1974). The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma, 14, 187–196.
Baker, S. P., & O’Neill, B. (1976). The injury severity score: An update. Journal of Trauma, 16, 882–885.
MacKenzie, E. J. (1984). Injury severity scales: Overview and directions for future research. American Journal of Emergency Medicine, 2(6), 537–549.
Olthof, D. C., Luitse, J. S., de Groot, F. M., & Goslings, J. C. (2013). A Dutch regional trauma registry: Quality check of the registered data. BMJ Qual Saf, 22(9), 752–758.
Boyd, C. R., Tolson, M. A., & Copes, W. S. (1987). Evaluating trauma care: The TRISS method. Trauma Score and the Injury Severity Score. Journal of Trauma, 27(4), 370–378.
Semmlow, J. L., & Cone, R. (1976). Utility of the injury severity score: A confirmation. Health Services Research, 11(1), 45–52.
Snaith R. P., & Zigmond, A. S. (1994). Hospital Anxiety and Depression Scale (HADS)—Experimentele Nederlandstalige versie ten behoeve van wetenschappelijk onderzoek.
Spinhoven, P., Ormel, J., Sloekers, P. P., Kempen, G. I., Speckens, A. E., & Van Hemert, A. M. (1997). A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological Medicine, 27, 363–370.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta psychiatrica Scandinavica, 67, 361–370.
Brom, D., & Kleber, R. J. (1985). De Schokverwerkingslijst. Nederlands tijdschrift voor psychologie, 40, 164–168.
van der Ploeg, E., Mooren, T. T., Kleber, R. J., van der Velden, P. G., & Brom, D. (2004). Construct validation of the Dutch version of the impact of event scale. Psychological Assessment, 16, 16–26.
Neal, L. A., Busuttil, W., Rollins, J., Herepath, R., Strike, P., & Turnbull, G. (1994). Convergent validity of measures of post-traumatic stress disorder in a mixed military and civilian population. Journal of Traumatic Stress, 7, 447–455.
Broadbent, D. E., Cooper, P. F., FitzGerald, P., & Parkes, K. R. (1982). The Cognitive Failures Questionnaire (CFQ) and its correlates. British Journal of Clinical Psychology, 21(Pt 1), 1–16.
Bridger, R. S., Johnsen, S. A., & Brasher, K. (2013). Psychometric properties of the Cognitive Failures Questionnaire. Ergonomics. doi:10.1080/00140139.2013.821172
Ponds, R., van Boxtel, M., & Jolles, J. (2006). De “Cognitive Failure Questionnaire” als maat voor subjectief cognitief functioneren. Tijdschrift voor Neuropsychologie, 2, 37–45.
WHOQOL group. (1996). WHOQOL-Bref. Geneva: WHO.
De Vries, J., & Van Heck, G. L. (1996). De Nederlandse versie van de WHOQOL-Bref [The Dutch version of the WHOQOL-Bref]. Tilburg: Tilburg University.
O’Carroll, R. E., Smith, K., Couston, M., Cossar, J. A., & Hayes, P. C. (2000). A comparison of the WHOQOL-100 and the WHOQOL-BREF in detecting change in quality of life following liver transplantation. Quality of Life Research, 9, 121–124.
Trompenaars, F. J., Masthoff, E. D., Van Heck, G. L., Hodiamont, P. P., & De Vries, J. (2005). Content validity, construct validity, and reliability of the WHOQOL-Bref in a population of Dutch adult psychiatric outpatients. Quality of Life Research, 14, 151–160.
De Vries J., & Van Heck G. L. (2003) Nederlandse handleiding van de WHOQOL. [Dutch manual of the WHOQOL].
Frommberger, U. H., Stieglitz, R. D., Nyberg, E., Schlickewei, W., Kuner, E., & Berger, M. (1998). Prediction of posttraumatic stress disorder by immediate reactions to trauma: A prospective study in road traffic accident victims. European Archives of Psychiatry and Clinical Neuroscience, 248(6), 316–321.
Yasan, A., Guzel, A., Tamam, Y., & Ozkan, M. (2009). Predictive factors for acute stress disorder and posttraumatic stress disorder after motor vehicle accidents. Psychopathology, 42(4), 236–241.
Ringdal, M., Plos, K., Lundberg, D., Johansson, L., & Bergbom, I. (2009). Outcome after injury: Memories, health-related quality of life, anxiety, and symptoms of depression after intensive care. Journal of Trauma, 66, 1226–1233.
Schnyder, U., Moergeli, H., Trentz, O., Klaghofer, R., & Buddeberg, C. (2001). Prediction of psychiatric morbidity in severely injured accident victims at one-year follow-up. American Journal of Respiratory and Critical Care Medicine, 164(4), 653–656.
Zeckey, C., Hildebrand, F., Pape, H. C., Mommsen, P., Panzica, M., Zelle, B. A., et al. (2011). Head injury in polytrauma—Is there an effect on outcome more than 10 years after the injury? Brain Injury, 25, 551–559.
Wallis, H., Renneberg, B., Ripper, S., Germann, G., Wind, G., & Jester, A. (2006). Emotional distress and psychosocial resources in patients recovering from severe burn injury. Journal of Burn Care & Research, 27(5), 734–741.
Holbrook, T. L., & Hoyt, D. B. (2004). The impact of major trauma: Quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. Journal of Trauma, 56, 284–290.
Toien, K., Myhren, H., Bredal, I. S., Skogstad, L., Sandvik, L., & Ekeberg, O. (2010). Psychological distress after severe trauma: A prospective 1-year follow-up study of a trauma intensive care unit population. Journal of Trauma, 69, 1552–1559.
Rivara, F. P., Jurkovich, G. J., Gurney, J. G., Seguin, D., Fligner, C. L., Ries, R., et al. (1993). The magnitude of acute and chronic alcohol abuse in trauma patients. Archives of Surgery, 128(8), 907–912.
Poole, G. V., Lewis, J. L., Devidas, M., Hauser, C. J., Martin, R. W., & Thomae, K. R. (1997). Psychopathologic risk factors for intentional and nonintentional injury. Journal of Trauma, 42(4), 711–715.
Soderstrom, C. A., Smith, G. S., Dischinger, P. C., McDuff, D. R., Hebel, J. R., Gorelick, D. A., et al. (1997). Psychoactive substance use disorders among seriously injured trauma center patients. Journal of the American Medical Association, 277(22), 1769–1774.
Michaels, A. J., Michaels, C. E., Smith, J. S., Moon, C. H., Peterson, C., & Long, W. B. (2000). Outcome from injury: General health, work status, and satisfaction 12 months after trauma. Journal of Trauma, 48(5), 841–848.
Livingston, D. H., Tripp, T., Biggs, C., & Lavery, R. F. (2009). A fate worse than death? Long-term outcome of trauma patients admitted to the surgical intensive care unit. Journal of Trauma, 67, 341–348.
Orwelius, L., Bergkvist, M., Nordlund, A., Simonsson, E., Nordlund, P., Backman, C., et al. (2012). Physical effects of the trauma and psychological consequences of preexisting diseases account for a significant portion of the health-related quality of life pattern of former trauma patients. Journal of Trauma, 72(2), 504–512.
Haagsma, J. A., Polinder, S., Toet, H., Panneman, M., Havelaar, A. H., Bonsel, G. J., et al. (2011). Beyond the neglect of psychological consequences: post-traumatic stress disorder increases the non-fatal burden of injury by more than 50%. Injury Prevention, 17(1), 21–26.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Delft-Schreurs, C.C.H.M., van Bergen, J.J.M., van de Sande, P. et al. A cross-sectional study of psychological complaints and quality of life in severely injured patients. Qual Life Res 23, 1353–1362 (2014). https://doi.org/10.1007/s11136-013-0546-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-013-0546-y